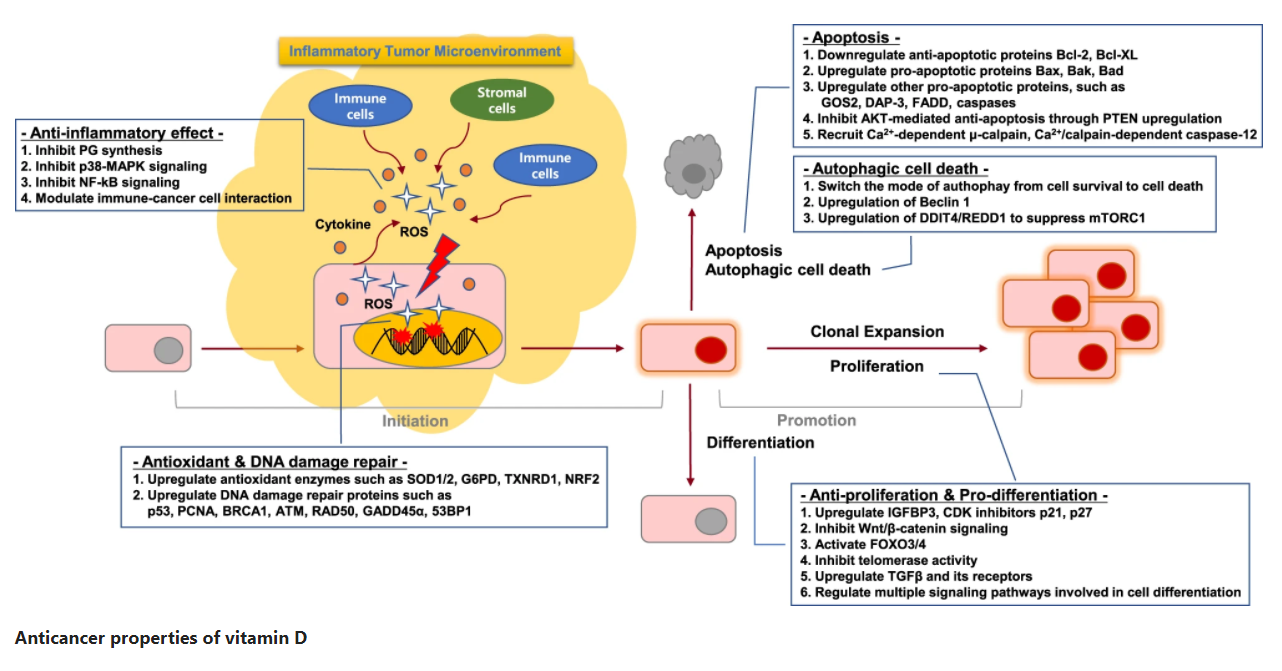
As mentioned earlier, vitamin D can regulate the entire process of tumorigenesis, including not only the initial stage of the tumor, but also the development stage of the tumor. Since the initial and developmental stages of tumors are critical to the growth of tumors, this article continues to discuss the various roles of vitamin D in the developmental stages of tumors.
Development Stage: Involved in Cell Proliferation/Differentiation and Apoptosis/Autophagy
Even in cells with gene mutations in the initial stage of tumors, vitamin D can still block the development of tumors by inhibiting cell proliferation, inducing cell differentiation and cell death, thereby exerting its anti-cancer properties.
Cell Proliferation and Differentiation
Vitamin D metabolites 20-OH-D3, 20-OH-D2, 1,20-(OH)2-D3 and 20,23-(OH)2-D3 can all inhibit tumor cell proliferation and induce tumor cell differentiation So as to play an anti-cancer effect. The anti-tumor cell proliferation properties of vitamin D are mediated by a variety of mechanisms, including the regulation of growth factors, cell cycle and signal pathways. Vitamin D inhibits retinoblastoma protein phosphorylation through the cyclin/cyclin-dependent kinase (CDK) complex, and blocks the transition of cells from the G0 phase to the G1 phase by inducing CDK inhibitors and inhibiting the c-MYC gene. In addition, vitamin D can also inhibit the Wnt/β-catenin signaling pathway by reducing the formation of transcription factor 4β (TCF4β) catenin complex or increasing the expression of Wnt antagonist Dickkopf-1 (DKK-1). In addition, vitamin D can increase the expression of forkhead transcription factor O3/4 (FoxO3/4), triggering the transcription of target genes involved in cell cycle arrest and anti-proliferation. Studies have also shown that vitamin D can induce the expression of transforming growth factor-β (TGF-β) and its receptors, and TGF-β is a strong inhibitor of epithelial cell proliferation. Similarly, in colon cancer cells, vitamin D The transformation of epithelial-mesenchymal cells can be weakened by TGF-β. In addition, the anti-proliferation and differentiation-inducing effects of vitamin D in tumor cells can also be achieved through the phosphoinositide 3-kinase/protein kinase B (PI3K/AKT), MAPK, NF-κB and Ca2+ signaling pathways.
Apoptosis and Autophagy
Vitamin D-induced apoptosis is mainly mediated by down-regulating the expression of anti-apoptotic proteins Bcl-2 and Bcl-XL and up-regulating the expression of pro-apoptotic proteins Bax, Bak, and Bad. In addition, there are also reports that vitamin D can initiate apoptosis events by recruiting Ca2+ -dependent apoptotic effectors. Vitamin D can also inhibit the AKT-mediated anti-apoptotic signaling pathway by increasing the expression of homologous phosphatase. Autophagy is a catabolic process that plays an important role in both cell survival and non-apoptotic cell death. More and more data show that in cancer cells, vitamin D can promote the transformation of cells from survival to death through autophagy, and can also induce cytotoxicity or static autophagy to enhance radiotherapy sensitization. Vitamin D-induced autophagic cell death can be attributed to the up-regulation of the autophagy-related gene beclin1. At the same time, CDK inhibitors may be involved in vitamin D-mediated autophagic cell death. In addition, vitamin D can also induce autophagy by inducing the expression of DNA damage-induced transcription factor 4 (DDIT4).
Vitamin D-based Cancer Treatment
Although there is still a lack of sufficient clinical randomized controlled trial data, some epidemiological, preclinical and in vitro experimental data indicate that activating the vitamin D signaling pathway may be the prevention and treatment of cancer A promising strategy. Therefore, some therapeutic interventions for vitamin D metabolism have been researched and developed for cancer treatment. Some scholars have found that vitamin D can enhance the effects of traditional anti-cancer drugs such as various antimetabolites and platinum drugs. Therefore, vitamin D has proven to be a promising candidate for combined chemotherapy. In addition, human resistance to drugs in tumor treatment is the main cause of tumor progression. Therefore, how to overcome drug resistance is currently the biggest challenge facing scientists. According to reports, vitamin D can increase the sensitivity of oral squamous cell carcinoma to cisplatin and the chemotherapy effect of breast cancer on tamoxifen. However, vitamin D-based cancer treatment has some potential limitations, so it should be considered when designing treatment strategies. One potential risk of the activation of the vitamin D signaling system is hypercalcemia, which may have a serious impact on the health of the body. In order to minimize the effects of hypercalcemia, researchers are working on the development of vitamin D receptor agonists, which are less effective in inducing hypercalcemia while maintaining a similarity anti-cancer activity to calcitriol. So far, nearly 1,500 vitamin D analogs have been tested for such effects, and a few compounds have been approved for further evaluation in clinical trials for leukemia, breast cancer, prostate cancer, and colon cancer. Therefore, understanding how vitamin D metabolism and signaling pathways are dysregulated in cancer will help to develop effective therapeutic drugs to overcome the limitations of the clinical use of vitamin D or its analogues.
