One of the characteristics that cancer cells can obtain and maintain in the body is their ability to evade detection and destruction by the human immune system. For example, some tumor cells produce higher-than-normal amounts of protein as a “don’t eat me” signal, which exists on the cell surface. These “don’t eat me” proteins are an immune checkpoint. They are “like the invisible cloak of cancer” and prevent white blood cells called macrophages from detecting, and engulfing.
CD24 and Cancer
The usual purpose of the “don’t eat me” signal is to prevent macrophages from attacking normal cells in the body. In the past decade, researchers have identified three other “don’t eat me” proteins, namely PD-L1, CD47 and B2M, which cancer cells use to escape macrophages. Most types of immunotherapies that have been used target white blood cells called T cells, which are a key component of the body’s second immune defense system (called adaptive immunity). In contrast, CD24-inhibiting macrophages are part of the innate immune system—the body’s first line of defense against infection and abnormal cells.
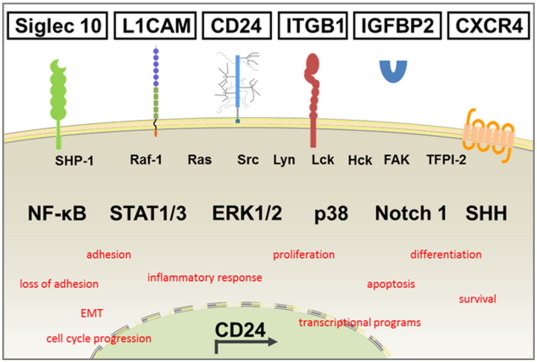
In a new study before, scientists discovered that a protein called CD24 is a new “don’t eat me” signal, which they believe is a potential target for cancer immunotherapy. The research team’s findings indicate that the well-known intractable ovarian cancer and triple-negative breast cancer are cancers that can be targeted for treatment by blocking CD24. Macrophages that infiltrate the tumor pass through a receptor called Siglec-10 Interact with CD24 to recognize the “don’t eat me” signal.
CD24 and COVID-19
In addition to CD24 can be used for cancer treatment, recent studies have found that it can also be used for the treatment of severely ill patients with new coronary pneumonia. In patients with mild and common symptoms of the new coronavirus, most of the damage to the human body is caused by the virus invading the lungs, intestines or other organs. However, in severely ill (and part of the general type) patients, many injuries are caused by the patient’s own excessive immune response. The new coronavirus has triggered an over-reaction of the immune system, causing the immune system to over-attack itself, causing a severe storm of inflammatory factors, and eventually death.
Therefore, drugs for the treatment of new coronaviruses can generally be divided into two categories, one is for the virus and the other is for inflammatory factors. The former are more antiviral treatments, which are generally used for mild and common patients, such as remdesivir, and monoclonal antibodies. Because severe stage treatment is the core point to calm the inflammatory factors, remdesivir and monoclonal antibodies have no effect on the severe disease. So what kind of medicine is generally used for severe Covid-19 illness? Dexamethasone, which is the only drug approved by the WHO to reduce mortality. Of course, the side effects of hormone drugs are also obvious. Besides, there is also tocilizumab. Tocilizumab can target interleukin 6 (an inflammatory factor secreted by white blood cells is responsible for the transmission of messages between immune cells). Since most of the human body’s immune response depends on interleukins, tocilizumab just targets this interleukin to eliminate inflammation. Therefore, it can also suppress the inflammatory factor storm caused by the new crown by targeting interleukin 6. However, it should be noted that these drugs themselves are not effective against the virus, and for patients who do not have an inflammatory factor storm, it will reduce their usual autoimmunity.
The recent Israeli study of the special drug “EXO-CD24” for the treatment of severely ill patients with new coronary disease also has a similar effect, mainly through the CD24 protein to reduce the immune response and eliminate the inflammatory factor storm. Among them, EXO-CD24 is a combination of CD24 protein and exosomes. CD24 can reduce the effect of the immune system, while exosomes are small lipid vesicles, which are mainly used as transport vehicles for CD24. The drug is inhaled through the nose and mainly acts on the patient’s lungs. The principle is to suppress the “immune storm” that is common in severely ill patients with new coronary disease, so that the immune system can clear the virus more safely. However, due to limitations in the number of patient studies, double-blind design, placebo group, and age distribution in this study, further studies are needed to determine the true efficacy of the drugs.
