Helicobacter pylori (HP) infection is the most common chronic infectious disease in the world, affecting approximately 4.4 billion people worldwide, but the prevalence varies greatly. HP can cause a variety of diseases, including gastric ulcers and twelve fingers intestinal ulcers, gastric mucosa-associated lymphoid tissue lymphoma (MALT) and gastric cancer, the International Agency for Research on Cancer lists HP as the first type of carcinogen. Gastric cancer is one of the five most common malignant tumors in the world and the third leading cause of death in the world Reason. Eradication of Helicobacter pylori has been proven to reduce the incidence of gastric cancer. Therefore, in order to treat Helicobacter pylori infection in a timely manner, accurate detection of Helicobacter pylori is essential. Here, we will continue to introduce the invasive detection method of Helicobacter pylori.
Endoscopy
In recent years, endoscopy technology has gradually matured and continuously improved, which makes it possible to use endoscopy to diagnose Hp infection. Some scholars believe that endoscopic manifestations such as gastric mucosal swelling, punctate erythema, variegated changes, fold enlargement, and muddy mucus can help diagnose Hp infection. In recent years, the observation of abnormal gastric mucosa through narrow-band imaging, confocal laser microendoscope and linkage imaging technology provides a basis for the diagnosis of Hp. Japanese endoscopy experts proposed that after Hp infection, under magnifying gastroscopy, it can be observed that the density of the veins in the gastric body collection decreases, and the texture becomes blurred, disordered, or even disappeared. Related studies have shown that observing the collecting veins of the gastric body has better specificity than observing the collecting veins of the gastric antrum. The narrow band imaging technique (NBI) diagnosis of Hp infection mainly observes gastric pits, which are tortuous, thick, and elongated, with obvious increase in branch curvatures, and interconnections in a dendritic shape. Confocal laser microscopy (CLE) provides gastric submucosal analysis and histological examination. CLE uses white and bright round spots, neutrophil infiltration, and crypt abscess as the diagnostic criteria for Hp infection, and the accuracy and specificity are more than 90%. Studies have shown that there is no Hp colonization in the metaplastic epithelium. CLE can identify goblet cells and small intestinal villi cells to determine whether there is local metaplasia and avoid biopsy at the metaplasia site, which affects the detection rate of Hp.
Rapid Urease Test-RUT
RUT is a detection method that can be performed in liquid or solid media, and there is no statistically significant difference in specificity between the two. RUT has the advantages of speed, simplicity and relatively high accuracy. However, RUT sensitivity is affected by the density and morphology of bacteria in the biopsy. Researchers believe that each biopsy specimen requires at least 104 microorganisms to reach the detection threshold of RUT, but a considerable proportion of patients may have a cell density below this limit and false negatives. In addition, treatment with PPIs, antibiotics, and bismuth agents may lead to false negative results. When the patient’s saliva is excessively secreted or the bile is refluxed to the stomach, it may contaminate the gastric biopsy specimen and cause a false positive result of RUT. The presence of other urease-producing bacteria in the stomach, such as Staphylococcus cephalosporium, may also cause false positive results.
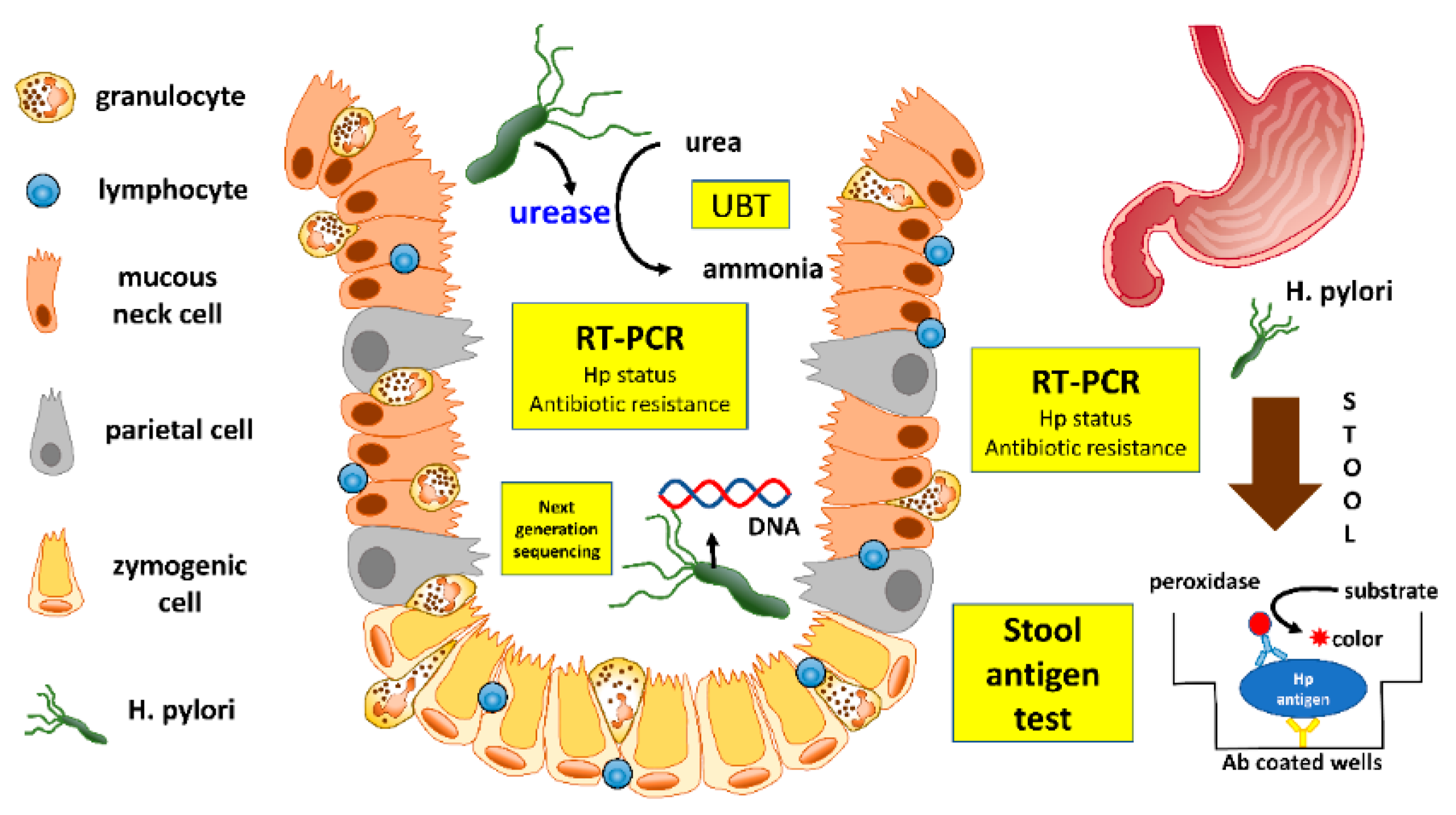
Polymerase Chain Reaction (PCR) Detection
PCR is not only used for bacterial detection, but also for broad-spectrum infection detection, new infection assessment, bacterial genotype identification, antibiotic resistance and epidemiological research. PCR detection of Helicobacter pylori has the advantages of simplicity, accuracy, rapidness, automation and efficiency. Accurate primer design and correct gene selection are the key to successful PCR reactions. Commonly used primers for Hp detection include 16srRNA, 23srRNA, CagA, VacA, ureA, ureB, ureC and Hsp60 genes. The test samples for Hp include fresh gastric mucosal tissue, tissue specimens that have undergone RUT, tissue specimens embedded in wax blocks, gastric juice, saliva, feces, and environmental samples. The researchers used fresh gastric mucosal tissue to perform PCR with 100% specificity and sensitivity, but the specificity of stool specimens was only 25%. The PCR and aniline blue staining of the tissues embedded in the wax block were compared, and the positive rate of Hp in the tissue wax block was 64.2%, which was higher than that of the aniline blue staining method. Because fixatives are needed in the process of tissue embedding, it may cause RNA fragmentation and is not suitable for RNA isolation, so there are some false negative results. With the completion of the whole genome sequencing of Hp, PCR technology is widely used in the diagnosis, genotyping, epidemiological investigation and prognostic judgment of Hp infection, and it has high clinical application value.
Stained Microscopic Examination of Tissue Sections
Histological examination is considered to be the gold standard for direct diagnosis of Hp in gastric mucosa. Scientists believe that the sensitivity and specificity of histological diagnosis of Helicobacter pylori are higher than UBT and RUT. In addition to directly observing rod-shaped and spherical bacteria, this detection method can also provide basic data on different types of gastritis, atrophy, dysplasia, metaplasia, and malignant tumors. At present, the more commonly used methods for detecting Hp include: Giemsa staining, H&E staining, W-S staining and immunohistochemical staining. In addition to directly observing the bacteria outside the body, H&E staining also helps to assess the severity of inflammation. However, the bacteria and the background in H&E staining are blue-purple, which is difficult to distinguish with the naked eye, and false negative results may be caused by the lack of experience of the observer. W-S staining is brown-black with silver stained particles attached to the bacteria, and the background is brown, which is easier to distinguish and has high sensitivity. However, too many silver-stained particles are often mixed with the bacteria, resulting in false positive results. The immunohistochemical staining of the bacterial body is brown, the background is blue, and the contrast is clear and easy to observe. But the disadvantage is that the reagents are expensive and the staining time is long. A sensitive detection study for the three detection methods found that the sensitivity and specificity of the three methods were H&E (94%, 97%), WS staining (97%, 98%), and immunohistochemistry (100%, 100%). Immunohistochemical staining has the highest sensitivity, specificity, and accuracy, and has low requirements for doctors to read the film. It is worthy of promotion in primary hospitals. The limitation of histological examination lies in the dependence on the sampler and the observer, and there are certain experience and ability requirements for staining techniques and identification of pathogens. In addition, the sensitivity of histology is often affected by the location, quantity and size of the biopsy tissue. The deformation of Hp caused by various factors reduces the recognition of conventional staining methods and causes false negative results.
Bacterial Culture Test
It is a challenging task to successfully isolate, extract and culture Hp from gastric biopsy specimens. Although Hp culture has extremely high specificity. However, due to strict culture conditions, Hp culture is less sensitive and the culture time is longer. Hp culture is affected by many factors, such as the quality of clinical specimens, the time interval between sampling and culture, and unsuitable transportation conditions (temperature, air exposure time, etc.). The sensitivity of cultured Hp from gastric biopsy specimens is above 90% and the specificity is 100% under optimal conditions. However, some researchers believe that even experienced experimenters can only cultivate the bacteria from 50% to 70% of the infected tissue. A large number of studies have shown that it is very difficult to cultivate Hp from feces, saliva and vomit because of the presence of symbiotic bacteria composed of other microorganisms that hinder the growth of Hp. Therefore, these methods are not recommended for clinical diagnosis.
