In recent years, with the changes in human environment and diseases, the incidence of fungal infections has been increasing year by year. Candida albicans is one of the important pathogens causing fungal infections. In addition, it is also an important food-borne pathogen.
Therefore, it is of great significance to carry out research on detection methods of Candida albicans in the fields of medical clinical testing and food safety testing.
Biological characteristics of Candida Albicans
Candida albicans exists widely in nature, and also exists in the oral cavity, upper respiratory tract, intestinal tract and vagina of normal people. It is generally small in number in normal organisms, does not cause disease, and is conditionally pathogenic. When the body’s resistance is reduced or the flora is out of balance, Candida albicans will multiply and change its growth form to invade human cells and cause diseases.
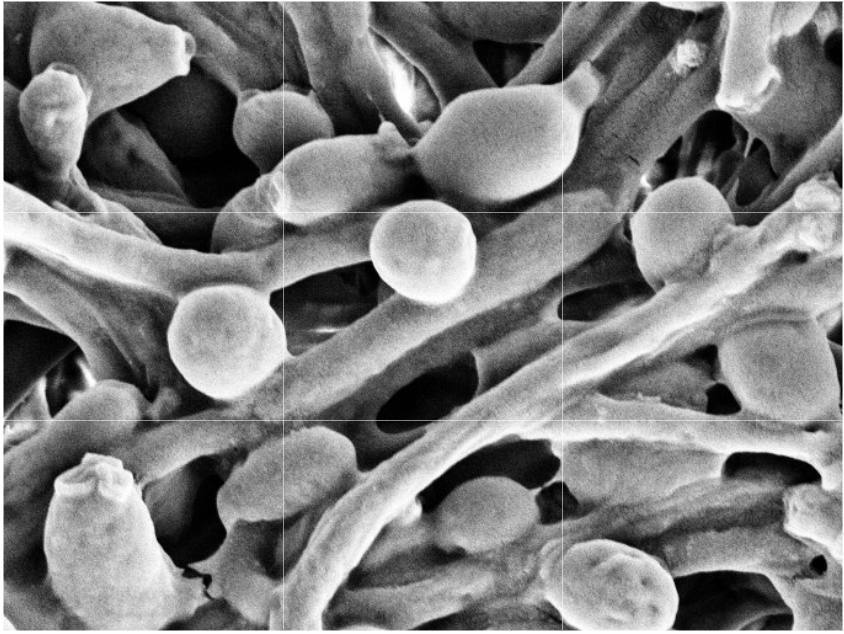
Figure 1. Candida albicans visualized using scanning electron microscopy.
The cells of Candida albicans were oval, and the cells of pathogenic strains showed pseudohyphae. The bacterium was incubated on blood agar or Sabouraud agar at 37°C or room temperature for 2 to 3 days to form gray-white cheese-like colonies. Microscopic examination of the smear showed oval blastocyte on the surface and many pseudohypha on the bottom layer. If inoculated on 4% maize agar and incubated at room temperature for 3-5 days, pseudohyphae, blastospores and chlamyspores can be seen. Candida albicans does not have strong resistance to heat, and it will die after 1 hour when heated to 60°C. But it is more resistant to drying, sunlight, ultraviolet rays and chemical agents.
Pathogenicity of Candida Albicans
Candida albicans causes superficial infection and deep infection. Related diseases caused by this species include skin candidiasis, including erosion between fingers (toes), which is more common in people who have been engaged in wet work for a long time. Candidal interacancerous rash is more common in Pediatric and obese hyperhidrosis, papular candidiasis more common in obese children, candidal paronychia, nail bed inflammation more common on the nails; mucosal candidiasis, including thrush more common in infants and young children, and genital candidiasis diseases; deep infection diseases include visceral candidiasis, which can affect all internal organs of the body, among which intestinal candidiasis and pulmonary candidiasis are more common. In addition, it can cause urethritis, nephritis, endocarditis and meningitis, and occasionally it can cause candida sepsis. Candida eruption, that is, skin allergy caused by Candida and its metabolites, the main damage is groups of sterile blisters, which are mostly seen between the fingers; psoriasiform, pityriasis rosea, seborrheic dermatitis,urticaria-like, centrifugal erythema annulare-like lesions can also be seen.
Factors Contributing to Candida Infection
Candidiasis is mainly acute, subacute or chronic infection caused by Candida albicans, and is the most common fungal disease. The clinical symptoms are complex and vary in severity, and children are mostly acute secondary infections. The disease often invades the skin and mucous membranes, and can also cause visceral or systemic infections. All visceral infections are often secondary to a variety of chronic wasting diseases, and there are predisposing factors such as long-term use of broad-spectrum antibiotics, corticosteroids, chemotherapy, and radiotherapy. In recent years, with the application of large doses of antibiotics, hormones, immunosuppressants, and the development of organ transplantation, its incidence has gradually increased, and it can be life-threatening and cause serious consequences. In addition to the yeast type causing superficial infections, so-called pseudomycelium is another morphological manifestation of yeast-like fungi. Germ tube and pseudomycelium production mainly occurs in patients with invasive infection. In addition, yeasts of the genus Candida are able to produce and secrete enzymes that allow facultative pathogenic microorganisms to penetrate vascular and mucosal barriers. Various bacteria of the genus Candida are generally transmitted through the pollution of dirt, and the main entrance is the nasopharyngeal passage, but fatty acids, acidic pH and hostile flora can also cause dysfunction of the skin surface to inhibit fungal infection, resulting in Superficial candidiasis. Invasive candidiasis spreads outward from the gastrointestinal tract after the bacteria infect the mucous membranes.
Candida Albicans Detection Method
Fungal testing methods include direct smear microscopy, fungal culture identification, fungal drug susceptibility testing, fungal infection tissue biopsy, fungal immunological tests, and molecular biology testing. Each method has its own advantages and disadvantages. direct microscopic examination is fast, direct, and low-cost, but the detection rate is low, which can no longer meet the clinical needs. Biopsy is very helpful for diagnosis, but this The method requires high technical level of clinicians and cannot be promoted in primary hospitals; although fungal culture is a diagnostic test for deep fungal infection, the positive rate of culture of this method is low, and in patients with disseminated candidiasis with negative blood culture It can be as high as 50%, so the diagnosis should be combined with the results of smear microscopy, tissue biopsy, serology and molecular biology tests; serological tests, such as 3-β-D glucan test (G test) and galactomannan test (GH test) are a new test technology developed in recent years and have been rapidly applied. The detection sensitivity and specificity are above 80%, so it becomes a supplementary inspection method for the diagnosis of Candida albicans; molecular biological testing is the most rapidly developed testing method in recent years, and some studies have used peptide nucleic acid fluorescence in situ hybridization ( PNA-FISH) has a sensitivity and specificity of 99%-100% and 100% for the detection of Candida albicans and/or Candida glabrata positive in blood culture, but due to various reasons such as cost, this method cannot be carried out vigorously. Therefore, fungal detection technology with lower cost and higher accuracy is urgently needed in the market and needs to be developed.
