Type 1 diabetes (T1DM) is an autoimmune disease caused by the destruction of beta cells, leading to the destruction of related pancreatic islet functions. In patients with this disease, both humoral and cellular immunity generally do not work properly. Among them, humoral immunity is mainly manifested by the presence of antibodies against self-substances in the patient’s body, mainly including anti-insulin antibodies, anti-tyrosine phosphatase antibodies, anti-islet cell antibodies, and anti-glutamate decarboxylase antibodies. These abnormal antibodies can damage The B cells that secrete insulin in the human pancreatic islet prevent it from secreting insulin normally.
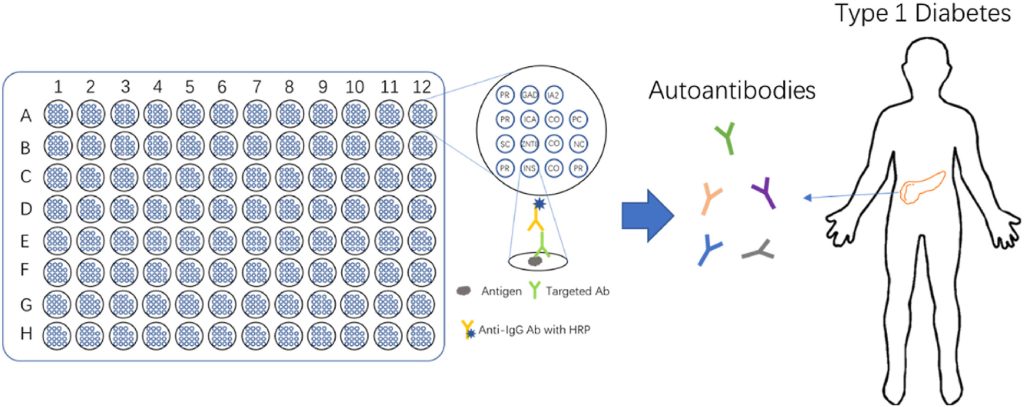
Figure 1. Improved diagnosis of type-1 diabetes mellitus using multiplexed autoantibodies ELISA array.
The Significance of Multiple Antibodies in Detecting T1DM
Anti-Islet Cell Antibodies
Among all the antigens, the most specific one is insulin. Many researchers have shown that there is not just one form of insulin in the body, but many that interact with the immune system. ZnT8 is a newly discovered antigen. All genes SLC30A8 are expressed in pancreatic antigens. The gene expression level of ZnT8 is relatively strong, ranking after insulin. As a high-risk patient group for T1DM, if the direct relatives of type 1 diabetes are positive for autoantibodies, the probability of developing the disease will be very high. Therefore, the incidence rate of immediate relatives is closely related to the type of positive antibodies.
Anti-Insulin Antibodies
Immediate relatives of mothers with type 1 diabetes are a special population for this type of disease. Some clinical studies have shown that whether a baby is positive for anti-insulin antibodies at birth does not affect the incidence of diabetes in children of mothers with type 1 diabetes later in life. When a baby is born, the probability of developing autoantibodies that are positive is lower than those that are negative, which is a protective effect. A long-term survey of patients with both partners suffering from type 1 diabetes found that the probability of their children being positive for antibodies is opposite to the probability of diabetes. The lower the probability of positivity, the higher the probability of developing diabetes. In this case, the rate of development is faster than that of one parent suffering from the disease.
Anti-Glutamic Acid Decarboxylase Antibody
In the general diabetes screening process, the detection of autoantibodies is still of great significance, although most patients with type 1 diabetes have no family history. Positive anti-glutamic acid decarboxylase antibodies are actually a higher risk factor in people without a family history of diabetes. The level of anti-glutamate decarboxylase antibodies is directly proportional to the risk of developing type 1 diabetes, with higher levels of the former associated with a higher risk of type 1 diabetes. There is a survey specifically focusing on children with diabetes. Among more than 100 cases in which children were positive for this antibody, 27 patients with type 1 diabetes had ZnT8A, anti-glutamate decarboxylase antibodies, and anti-insulin antibodies. The probability of antibodies in patients before onset of disease is between 60% and 80%, and some patients have anti-glutamic acid decarboxylase antibodies and anti-insulin antibodies turning negative.
Diagnostic Significance of Multiple Antibodies for Type 1 Diabetes
Among patients with T1DM, race, disease course, and age at onset can largely affect the probability of positive occurrence of islet autoantibodies. There are two types of joint detection of autoantibodies: single detection and multiple detection. The latter is commonly used in the detection of T1DM, while the sensitivity of the former is relatively low. If only anti-islet cell antibodies are present, the risk of developing diabetes is only about 5%. If multiple antibodies are present at the same time, the incidence rate can reach up to 66.2%. In the case of the simultaneous presence of multiple antibodies, anti-islet cell antibodies, anti-tyrosine phosphatase antibodies or (and) anti-glutamate decarboxylase antibodies have the highest prevalence when these two or three antibodies are combined together. Various reasons such as gender, age, environment, race, and genes can lead to positive antibody production in patients with type 1 diabetes. Anti-glutamic acid decarboxylase antibodies are highly likely to be positive and stable in new-onset patients with type 1 diabetes. The probability of GAD65A being positive in boys under 10 years old is not high. As age increases, the probability of onset in older age groups, such as adolescence, is as high as 80%, and whether it is positive or not at this age is related to Gender doesn’t matter. The probability of positive anti-islet cell antibodies is higher than that of anti-glutamic acid decarboxylase antibodies. This is because adolescents mainly have anti-islet cell antibodies in the early morning, and this anti-islet cell antibody is negatively correlated with age. One of the main target antigens of anti-islet cell antibodies is IA-2. The probability of this target antigen being positive in patients is between 30% and 70%.
Although immediate relatives of type 1 diabetes are at high risk for developing diabetes, these high-risk individuals only account for about 13% of all disease-causing people. So many people with type 1 diabetes have no family history of the disease. According to the survey of newly diagnosed patients, IA-2A is positive in all patients with type 1 diabetes. Through this survey, it can be found that the longer the disease history, the lower the probability of being positive. But anti-aging glutamate decarboxylase does not have this feature. Anti-insulin antibodies, this type of antibody is most affected by age. Because there are many factors that affect this condition. If a single autoantibody is detected, neither the sensitivity nor the required specificity of the test can achieve satisfactory results. Therefore, multiple autoantibody tests are now generally used in the medical community, which greatly avoids the risk of a single autoantibody test.
The Relationship Between Multiple Antibodies
When studying the direct relationship between various antibodies and type 1 diabetes, many studies have shown that these antibodies actually have a certain relationship with each other. For example, the order in which antibodies appear in the human body has a certain pattern. According to the survey data and experience accumulated by experts over the years, it can be found that among various antibodies, anti-glutamic acid decarboxylase and anti-insulin antibodies appear relatively first. Although there have been many studies on these antibodies, there is currently no clear and unified conclusion, and some conclusions are even contradictory to each other. Therefore, it takes time to make a more unified and accurate judgment on the relationship between these antibodies.