What Is the “Oxygen Pathway”?
The oxygen-sensing pathway actually refers to every cell in the human body, and it can sense how much oxygen is in the environment in which it lives.
Oxygen is vital to animal life: mitochondria in almost all animal cells use oxygen to turn food into useful energy. Otto Warberg revealed that this conversion is an enzymatic process. During the evolution process, the body evolved a protective mechanism to ensure that the tissue and cells have sufficient oxygen supply. The carotid body is adjacent to the large blood vessels on both sides of the neck. It has been found that it contains special cells that can sense the oxygen content in the blood. Interestingly, the blood oxygenation of the carotid body can communicate directly with the brain to control the respiratory rate. In addition, in addition to the carotid body control to adapt to low oxygen levels (hypoxia), there are other basic physiological adaptations. Clinical studies have found that a key physiological response to hypoxia is elevated levels of erythropoietin (EPO), which increases red blood cell production. The importance of hormone-controlled erythropoiesis was known at the beginning of the 20th century, but how the process itself is controlled by oxygen remains a mystery.
To understand this mystery, Gregg Semenza studied the EPO gene and how it is regulated by different oxygen levels. By genetically modified mice, it was found that specific DNA fragments located next to the EPO gene mediate responses to hypoxia. The study found that the oxygen sensing mechanism is not only present in kidney cells that normally produce EPO, but in almost all tissues. These important findings indicate that the mechanism is ubiquitous and play a role in many different cell types. In order to find out the cellular components that mediate this response, the researchers conducted further exploration. Eventually they found a protein complex in the cultured hepatocytes that binds to the DNA fragment in an oxygen-dependent manner. This complex is called hypoxia inducible factor (HIF). In 1995, Semenza began extensive research on HIF complexes and published important findings, including the identification of genes encoding HIF. Hypoxia-inducible factors were found to contain two different DNA-binding proteins, the so-called transcription factors, now called HIF-1α and ARNT.
Oxygen Pathway Mechanism
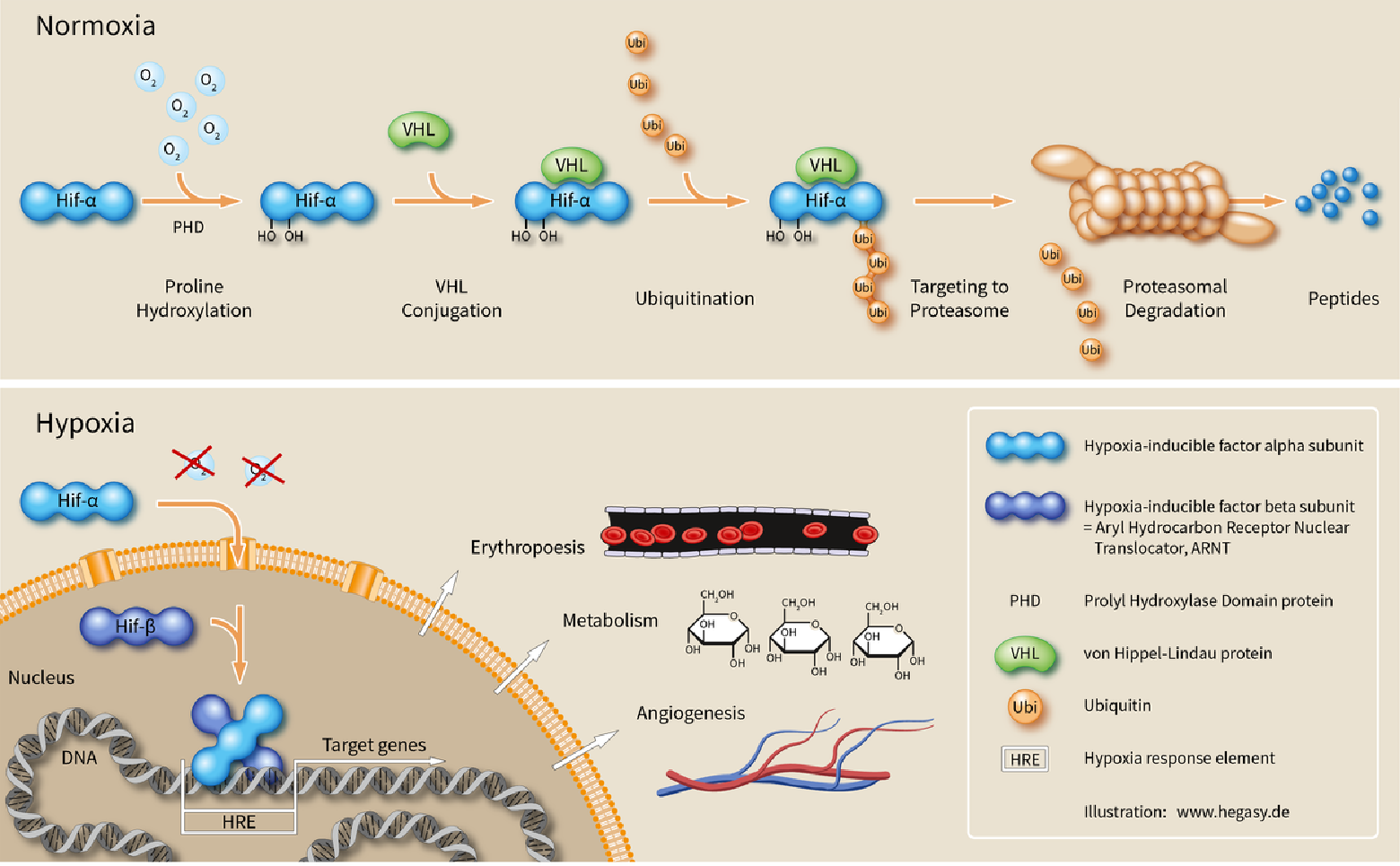
The study found that when the oxygen level is high, HIF-1α cannot be stably present, and the cells contain almost no HIF-1α. However, when the oxygen content is low, the amount of HIF-1α is increased, so that it can bind and regulate the EPO gene as well as other genes having HIF-binding DNA fragments. In addition, the cause of instability of HIF-1α under oxygen-containing conditions was also found. At normal oxygen levels, a cellular machine called the proteasome degrades HIF-1α. Under these conditions, the HIF-1α protein is labeled with ubiquitin. This marker can be recognized by the proteasome to degrade the target protein. How does ubiquitin combine HIF-1α in an oxygen-dependent manner? The answer comes from an unexpected direction. While Semenza and Ratcliffe explored the regulation of the EPO gene, cancer researcher William Kaelin, Jr. is studying a genetic syndrome, von Hippel-Lindau disease (VHL disease). This genetic disorder causes a dramatic increase in the risk of certain cancers in families with hereditary VHL mutations. Kaelin showed that the VHL gene encodes a protein that prevents cancer attacks. It has also been shown that cancer cells lacking the functional VHL gene express abnormally high levels of hypoxia-regulated genes. However, when the VHL gene was reintroduced into cancer cells, normal levels were restored. This is an important clue that VHL is involved in some way in controlling hypoxic responses. Ratcliffe and his team made a key finding: prove that VHL can physically interact with HIF-1α and is required for degradation at normal oxygen levels.
The Meaning of Oxygen Pathway
The cell’s perceived oxygen concentration is closely related to various normal physiological activities, such as embryonic development and exercise. Without this oxygen-sensing pathway, cells can’t make a clear adjustment to the body’s behavior, including the outside world and the internal environment, so it’s very important to the body.
In addition, the mechanism’s elaboration helps to understand some diseases or developmental mechanisms. For example, in some cancer cells or during embryonic development, these cells are hypoxic due to their rapid growth, which activates the sensory signaling pathway. The activated pathway causes a series of changes in the body, including allowing the cells to secrete some factors to promote the formation of new blood vessels and obtain oxygen, and also promote the cells to survive. Without this signaling pathway, once hypoxic, cells can die or enter an unhealthy state. Therefore, whether it is normal physiology or disease, this signaling pathway is very important for cells.
